Introduction: Immune thrombocytopenia (ITP) is an acquired autoimmune disease characterized by isolated thrombocytopenia and varying degrees of bleeding symptoms. Platelets are anucleate cytoplasmic cell fragments that play dual physiological roles as both cellular mediators of thrombosis and immune modulatory cells. Platelets are the largest storage pool of TGF-β1, a crucial enforcer of immune homeostasis and tolerance. Studies have shown that TGF-β1 released by platelets contributes to the pathogenesis of pulmonary arterial hypertension and cervical carcinoma. Myeloid-derived suppressor cells (MDSCs) are a heterogeneous group of immature myeloid cells with potent immunosuppressive functions. Our previous studies have shown that MDSCs are impaired in number and function in patients with ITP. The objective of this study was to elucidate the underlying molecular mechanisms of MDSCs reprogramming by platelet-derived TGF-β1.
Methods: A transwell assay was used to determine the impact of platelets on MDSCs induced from peripheral blood mononuclear cells (PBMCs) of ITP patients and healthy controls. The percentage of circulating MDSCs in ITP patients was detected before and after administration of thrombopoietin receptor agonists (TPO-RAs). Besides, anti-CD61 immune-sensitized splenocytes were transferred into SCID mice to establish an active murine model of ITP. Subsequently, MDSCs from TPO-RA-treated ITP mice were transplanted as cell therapy to rescue treatment-free ITP mice. In specific, adeno-associated viral (AAV) vectors efficiently infected MDSCs to enable cell-specific Smad2/3 knock-down. Finally, platelet specific TGF-β1-deficient mice were used to validate the effect of platelet-derived TGF-β1 on MDSCs.
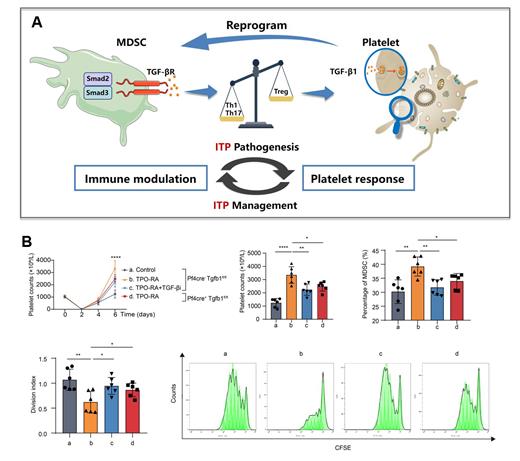
Results: TGF-β1 levels in the supernatant of MDSCs co-cultured with platelets of high concentration was significantly higher than that in MDSCs co-cultured with platelets of low concentration or alone. FACS analysis showed that platelet mass enhanced the inhibitory effects of MDSCs on the proliferation of CD4 + T cells, which could be offset by TGF-β1 inhibitor (TGF-βi). Besides, TPO-RAs treatment induced significantly increased percentage of circulating MDSCs in responders with chronic ITP. Likewise, TPO-RA significantly expanded MDSC population in active ITP murine models. Furthermore, after receiving donor MDSCs from TPO-RA-treated ITP mice, arrested differentiation of plasma cells, reduced Fas ligand expression on cytotoxic T cells, and re-balanced T cell subsets were found in the recipient mice, indicating augmented inhibitory functions of MDSCs. Mechanistically, transcriptome analysis confirmed the participation of TGF-β/Smad pathway in donor MDSCs from TPO-RA-treated ITP mice, which was offset by Smad2/3 knockdown. Finally, by constructing ITP models using Pf4 cre-Tgfb1 fl/fl and Pf4 cre+Tgfb1fl/fl mice, we found that TGF-β1 inhibition and platelet TGF-β1-deficence, both, could counteract the elevated platelet count and MDSCs percentage, as well as improved immunosuppressive capacity of MDSCs trigged by TPO-RA modulation.
Conclusion: To sum up, it was demonstrated that platelet TGF-β1 induced the expansion and functional reprogramming of MDSCs via TGF-β/Smad pathway. These data indicate that platelet recovery not only serves as an endpoint of remission, but also paves the way for tolerance induction in immune-mediated thrombocytopenia. Our exploratory study deciphered immunological changes induced by TPO-RAs and helped to identify molecular mechanisms responsible for long-term remission after TPO-RA discontinuation.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal